Diabetes Care and Education Resources
This category page brings together practical reading on Diabetes for patients and caregivers.
It covers everyday terms, common symptoms, and care-planning topics that often come up in visits. It also links to telehealth guides and condition collections across Medispress. Use it to compare topics, learn key language, and prepare better questions.
Care is provided by licensed clinicians in the United States.
Diabetes: What You’ll Find
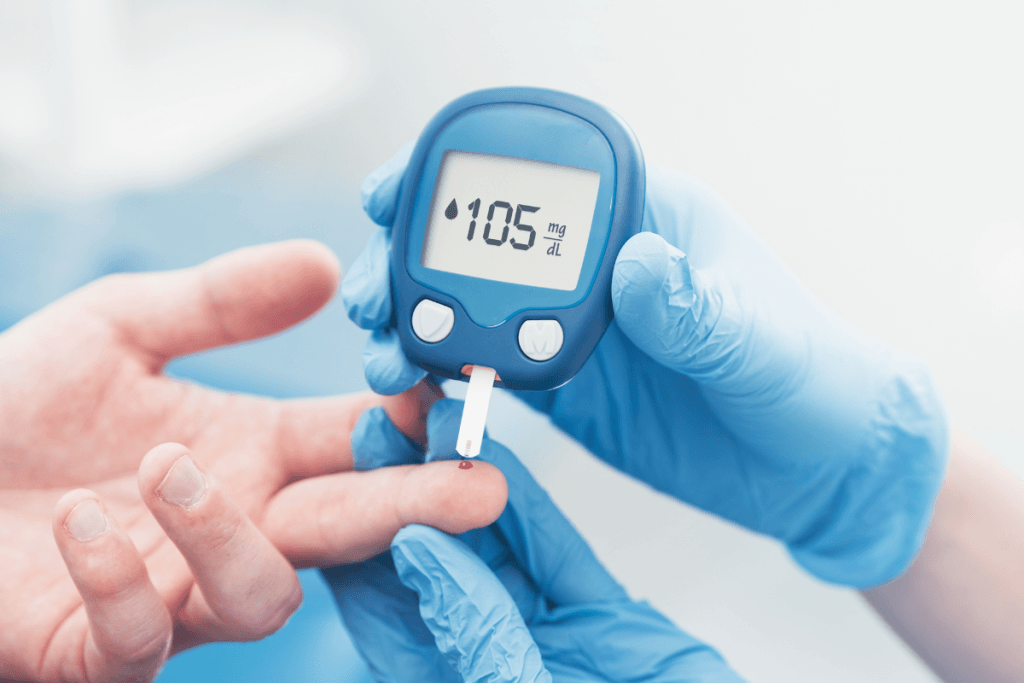
This collection focuses on day-to-day realities of living with blood sugar concerns. It includes explainers that clarify what different care paths may involve. It also highlights common tools, like glucose meters and continuous glucose monitoring (CGM).
Several posts cover how virtual care fits into chronic condition check-ins. See Manage Blood Sugar With Ease for a practical overview. For broader scope, review What Telehealth Can Treat and Telehealth For Family Healthcare.
Quick tip: Keep a running list of medicines, supplements, and refills.
- Plain-language definitions for common blood sugar terms
- Medication and insulin basics, written at a high level
- Monitoring options, including CGM and fingerstick meters
- Lifestyle topics, like meals, movement, and sleep routines
- Complication awareness, like eye and foot concerns
- Telehealth logistics, including setup and visit flow
Some guides focus on access barriers and practical planning. If reliable internet is a challenge, Benefits Of Telehealth In Rural Areas offers helpful context.
How to Choose
Start by matching resources to the situation at hand. Many people begin with the condition collection for Type 2 Diabetes, then branch into monitoring and medication topics. Others begin with lifestyle planning or visit preparation, especially after a new lab result.
Match topics to the situation
- New diagnosis versus ongoing follow-up questions
- Prediabetes questions versus established glucose control concerns
- Pregnancy-related blood sugar concerns and postpartum follow-up planning
- Pediatric needs, including school routines and caregiver coordination
- Monitoring approach, including meter logs versus CGM reports
- Current medicines, including insulin products and non-insulin options
- Side effects, adherence barriers, and refill coordination challenges
- Complication screening topics, like eye checks and foot checks
Plan questions for a visit
Virtual visits go better with a short agenda and clear notes. Use Top Telehealth Visit Questions to structure key talking points. Review Prepare For Telehealth Appointment to organize basics like allergies and prior records.
Why it matters: A clean summary reduces back-and-forth during a time-limited visit.
Tech hiccups can distract from important details. Tech Troubles Tips covers practical setup steps for smoother calls.
Visits take place by video inside our HIPAA-secure app.
Safety and Use Notes
Blood sugar swings can feel scary, especially when symptoms appear suddenly. Hypoglycemia and hyperglycemia can share early signs like shakiness or fatigue. Symptoms can also look different across ages and pregnancy. For a neutral symptom overview, see this CDC overview.
People with type 1 diabetes often need tighter planning around insulin access and supplies. Storage, injection technique, and sick-day planning can all affect safety. Non-insulin medicines can also carry risks, including dehydration or stomach side effects. For low-blood-sugar safety basics, see ADA guidance.
- Know which medicines must not be stopped abruptly without clinical input
- Check for interaction risks with alcohol, supplements, and new prescriptions
- Watch for signs of neuropathy (nerve damage), like burning or numbness
- Take vision changes seriously, including sudden blur or new floaters
- Inspect feet for sores, swelling, or skin breakdown between visits
- Use extra caution with driving if symptoms can come on quickly
This section supports education and safer conversations. It does not replace personalized medical guidance.
Access and Prescription Requirements
Many glucose-lowering medicines and supplies require a valid prescription. Pharmacies and clinicians may need to confirm identity and review medication history. Some items also require additional documentation, depending on the product category. Administrative steps help reduce errors and mismatched therapies.
For Diabetes-related medication questions, clinicians may review current medicines and recent trends. They may also discuss whether an in-person evaluation is needed first. Some people use cash-pay options, often without insurance, when coverage is limited.
- Prescription-only items require clinician authorization and pharmacy verification
- Controlled substances follow stricter rules and may have added limits
- Refills can depend on prior records and the clinical context
- Some devices may require compatibility checks or documentation
When clinically appropriate, clinicians can route prescriptions through partner pharmacies.
Related Resources
For broader navigation beyond this category page, browse Diabetes Prevention And Management for aligned services and resources. Several telehealth posts also explain what a virtual visit can and cannot cover. That context helps set expectations and reduce surprises.
Some readers also look for general chronic-care planning. Start with Why Telehealth Works For Everyone for a big-picture view. If access barriers are a concern, Telehealth And Indigenous Communities adds helpful perspective.
This content is for informational purposes only and is not a substitute for professional medical advice.

November 3, 2025
7-Day Meal Plan for Gestational Diabetes That Works
Getting a gestational diabetes diagnosis can make meals feel complicated overnight. You may be tracking numbers, reading labels, and second-guessing cravings. A structured 7-day meal plan for gestational diabetes can…

October 31, 2025
How To Prevent Gestational Diabetes With Daily Habits
Pregnancy changes how your body handles sugar (glucose). For some people, those changes lead to higher-than-expected blood sugar during pregnancy, called gestational diabetes. Learning how to prevent gestational diabetes starts…

September 22, 2025
How To Get Mounjaro For Weight Loss Safely: Key Steps
Interest in GLP-1–based medicines has grown fast. Many people want clear, safe information before they act. If you are researching how to get Mounjaro for weight loss, it helps to…

September 17, 2025
Can You Reverse Type 2 Diabetes With Lifestyle Changes
Many people hear “type 2 diabetes” and immediately wonder: can you reverse type 2 diabetes? The honest answer is nuanced. There is no single, permanent “cure” that fits everyone. But…

September 15, 2025
7-Day Meal Plan for Prediabetes With Simple, Steady Meals
Prediabetes can feel confusing at first. You may hear “cut carbs” and “eat better,” but get few specifics. A practical 7-day meal plan for prediabetes helps you make fewer daily…

September 1, 2025
Mounjaro vs Ozempic: Key Differences For Diabetes And Weight
If you’re weighing options for type 2 diabetes care or weight management, you’ve probably seen the Mounjaro vs Ozempic comparison. The names show up in headlines, social feeds, and clinic…

August 11, 2025
Benefits Of Ozempic For Weight Loss And Diabetes: Basics
Ozempic (semaglutide) often comes up when weight and blood sugar overlap. It is a prescription medicine for type 2 diabetes. Some people also use it off-label for weight management under…

July 7, 2025
Signs of Hypoglycemia: How to Recognize and Respond
Low blood sugar (hypoglycemia) can feel sudden and unsettling. It can also be easy to misread as stress, hunger, or poor sleep. Learning the signs of hypoglycemia helps you respond…

June 30, 2025
Signs of Hyperglycemia: Symptoms and When to Get Care
High blood sugar can build quietly, then suddenly feel overwhelming. Knowing the signs of hyperglycemia helps you act sooner, whether you live with diabetes, have prediabetes, or are simply feeling…

May 19, 2025
Reverse Prediabetes: Practical Steps for the Next 90 Days
Hearing “prediabetes” can feel like a warning siren. It’s also a real opportunity. For many people, early changes in food, movement, sleep, and follow-up testing can improve blood sugar and…
Frequently Asked Questions
What can be found on this Diabetes category page?
This page collects educational posts and browsing links related to blood sugar concerns. Topics often include monitoring tools, medication basics, insulin concepts, lifestyle planning, and complication awareness. It also includes telehealth preparation guides, like how to plan questions and avoid tech issues. Some links lead to condition collections that group related options. The goal is clearer navigation and better understanding, not personalized treatment advice.
How do I decide which topic to read first?
Start with the question that feels most urgent or confusing. Some people begin with symptoms and basic definitions to reduce uncertainty. Others begin with monitoring choices, like CGM versus fingerstick meters. If a visit is coming up, telehealth preparation content can help organize notes and priorities. If the goal is understanding a specific condition type, use the condition collection links for a more focused path.
Can Medispress help with virtual care for blood sugar concerns?
Medispress offers video telehealth visits through a secure, HIPAA-compliant app. Licensed clinicians in the United States provide care during these appointments. When it is clinically appropriate, a clinician may coordinate prescription options through partner pharmacies. Some concerns still require in-person exams or urgent evaluation. This category page supports learning and planning, so the visit time can focus on the main issues.
What information is helpful to have ready for a telehealth visit?
A short medication list helps, including doses, timing, and recent changes. Many people also prepare recent blood sugar readings, trends, and notable symptoms. Include allergies, past reactions, and any relevant diagnoses from prior care. If using a glucose meter or CGM, having a summary report can save time. It also helps to write three to five questions in priority order.
When are low or high blood sugar symptoms urgent?
Some symptoms need urgent assessment, especially if severe or fast worsening. Examples include confusion, fainting, seizures, chest pain, trouble breathing, or signs of stroke. Persistent vomiting, severe dehydration, or inability to keep fluids down can also be serious. People who are pregnant, very young, or frail may need extra caution. For immediate danger, emergency services are appropriate. Educational content cannot replace emergency care decisions.